CHARBONNEAU: Ventilator treatment for COVID-19 leads to questions of end-of-life
NOW IS THE TIME TO TALK to your friends and family about your prospects of survival should you become deathly ill. But if you’re like me, you’d rather not start the conversation.
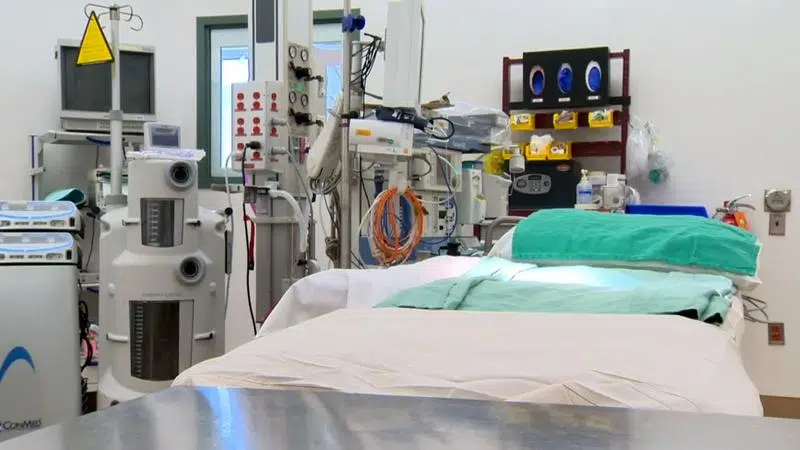
If you are unfortunate enough to catch the new coronavirus and are placed on a ventilator, the odds are two-to-one that you will die. And if you survive, your quality of life could be seriously compromised.
The numbers are still coming in, but they don’t look good. One review conducted in China said that 86 percent of COVID-19 patients put on ventilators eventually died. In the UK, about two-thirds of ventilated patients died.
From an optimistic perspective, you have a chance of living so why not take it?


