Kamloops doctor wants other addiction treatments used before heroin compassion clubs
KAMLOOPS — As British Columbia grapples with an ongoing overdose crisis, alternative solutions are now being considered to combat drug-related fatalities.
The BC Centre on Substance Use is proposing selling legally regulated heroin to reduce the amount of deaths coming from a toxic drug supply.
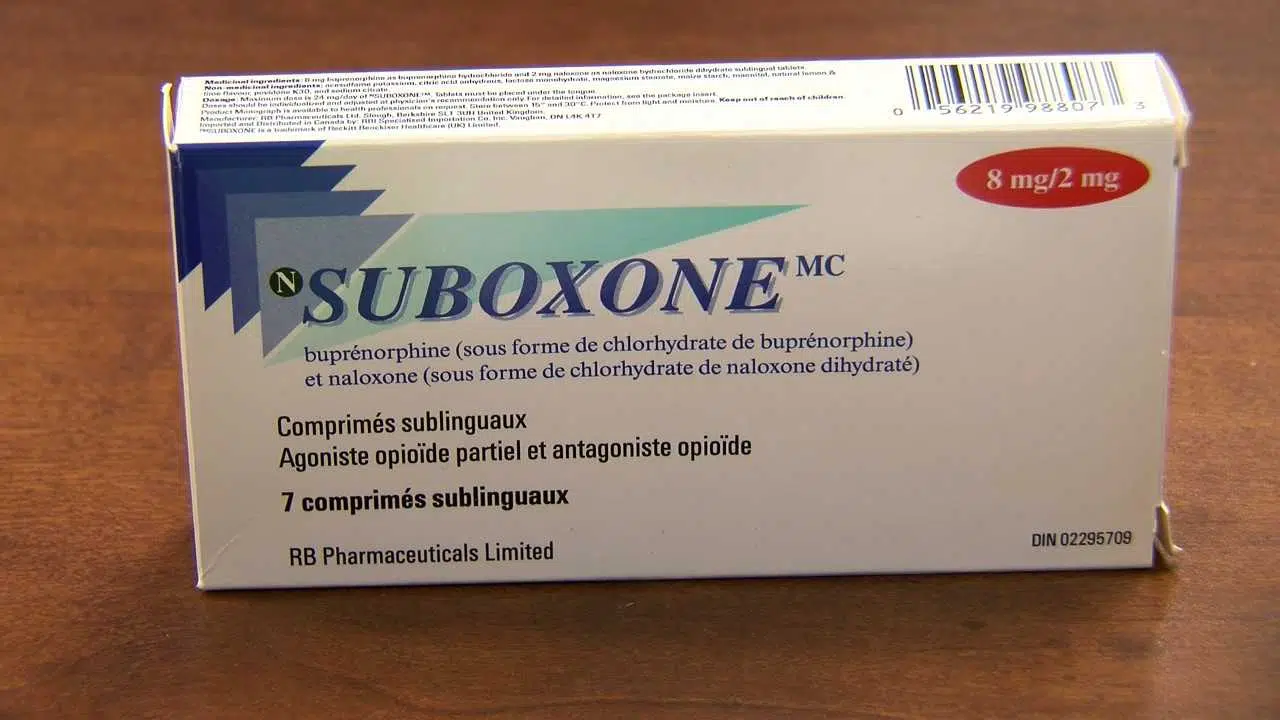
Medical professionals in Kamloops have varying opinions on the practice, along with the idea of injectable opioid agonist treatment (iOAT) — brought about by Kelowna opening an iOAT clinic in April.


