Lack of family doctors still among big gaps in health care
KAMLOOPS — The lack of family doctors is a health care challenge that is not going away. But what can be done to remedy the problem?
The provincial government introduced the ‘GP for Me’ program in 2010, aiming to find every B.C. citizens a family physician by 2015. That has yet to happen.
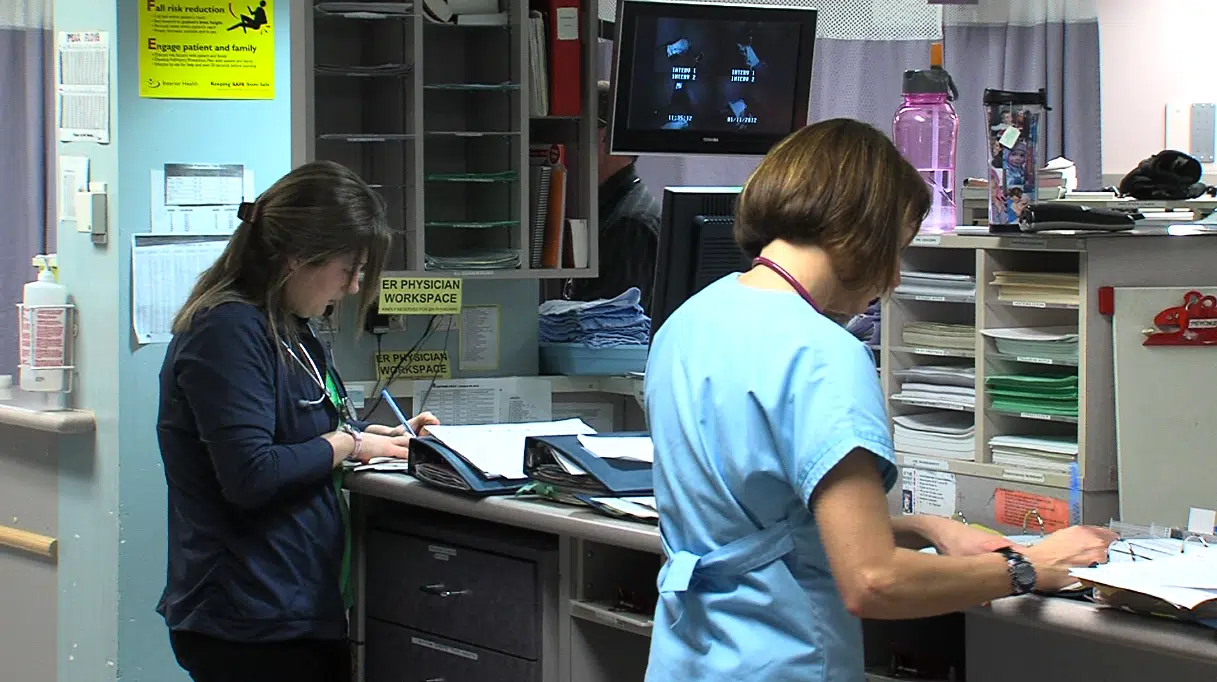
On Wednesday in Kamloops, a Standing Committee on Health met to hear from professionals in the field to see what can be done to improve the situation.


